Vasectomy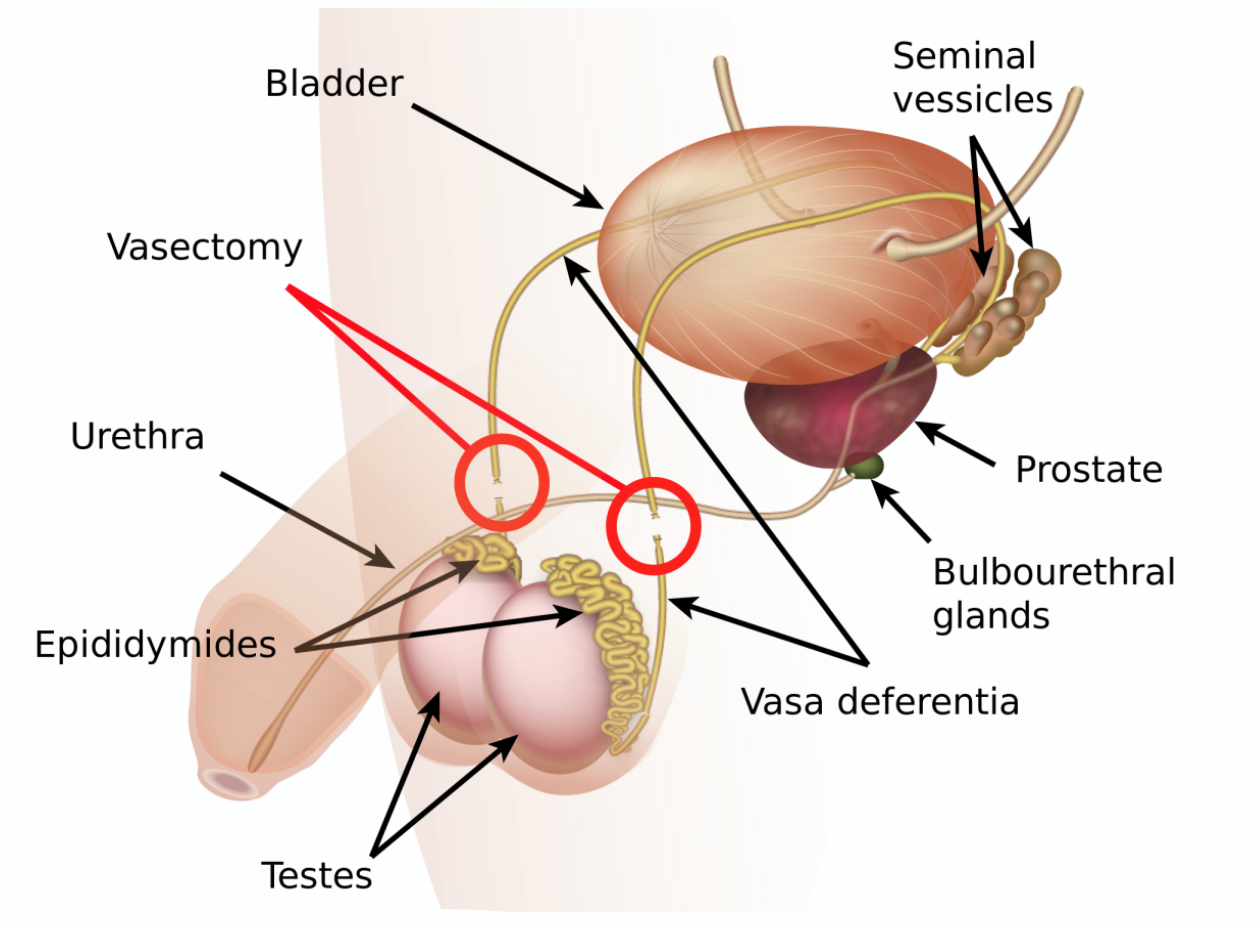
This means permanently stopping the flow of sperm from the testicles to the outside, thus preventing a man from fathering children. The operation may occasionally also be used to prevent urine from refluxing along the vas and may be used to treating recurrent infection of the tubules near and inside the testicle (epididymo-orchitis) where non-surgical options have failed.The scrotum may be shaved before being cleaned with antiseptic. Under local or general anaesthetic, the sperm tube (vas deferens) is located on each side and a small cut made in the scrotum, so the vas can be seen. The tubes are cut, and the cut ends tied with non-absorbable sutures. A length of each tube may be removed. The inner lining of the tubes may be burnt with an electrical current to seal them, and the ends buried beneath loose tissue. Both sides are usually treated in the same way.The choice of procedure depends on the surgeon. Any bleeding is stopped, and the separate ends of the cut tubes are replaced in the scrotum. The skin may be closed with fine absorbable stitches if necessary.
RISKS
These are the commoner risks. There may be other unusual risks that have not been listed here. Please ask you surgeon if you have any general or specific concerns.
There are risks associated with any anaesthetic.
You may have side effects from any drugs used. The commoner side effects include light-headedness, nausea, skin rash and constipation.
A vasectomy has the following specific risks and limitations:
- During the operation, you may notice a slowed heart beat and may feel faint.
- After the operation, you may develop a bruise in the scrotum that may take several weeks to get better.
- You may develop an infection in the skin wound that may need antibiotic treatment.
- Your partner and you will need to use alternative contraceptive methods for at least 3 months until your ejaculate samples have been tested and you have been told they are clear of sperm.
- There is always a small chance your ejaculations will never clear of sperm due to technical failure. This will require a repeat operation.
- There is a remote chance the vas may re-join spontaneously, even after you have been sterile for some time (re-canalisation). If this happens, you may no longer be sterile.
- Despite this, you should regard the operation as permanent. Reversals can be done, but they are expensive and are not always successful. THEY ARE NOT COVERED BY MEDICAL AID.
- You may develop a generally painful and swollen area at the back of a testicle and this may persist for some months (congestive epididymitis). This can be treated with scrotal support, ice packs and anti-inflammatory tablets.
- You may develop small cysts at the back of the testicle (epididymis cysts).
- You may develop small inflammatory nodules (sperm granulomas) around the cut ends of the vas or in the epididymis. These are unlikely to cause symptoms, but uncommonly result in some tenderness or pain with ejaculation. Most respond to simple treatments if necessary.
- There is a small risk you may develop long term aching in the testicles (post-vasectomy syndrome). This is usually mild and responds to anti-inflammatory medication. In a few men, this can be persistent.
- Rarely, a connection may form between a cut vas and your skin (vasocutaneous fistula). This requires surgical treatment.
- Although a couple of studies suggested men may have an increased risk of prostate cancer after a vasectomy, many other studies have not found any association.
Some of the above risks are more likely if you smoke, are overweight, diabetic, have high blood pressure or have had previous heart disease.
When you are discharged, take care of the following:
- Take it easy for the first 2 days after the procedure to minimise the risk of bleeding and bruising
- Wear firm-fitting underwear to help minimize bleeding
- You can remove your dressing/plaster after 2 days
- Sexual activity can be resumed after 1 week if you are comfortable
- Finish all prescribed medication
- Remember to do your Post Vasectomy follow-up semen analysis 3 months after your procedure. (drop off at Ampath pathologists)
- Contact your doctor if you have severe pain, bleeding or fever
