TURP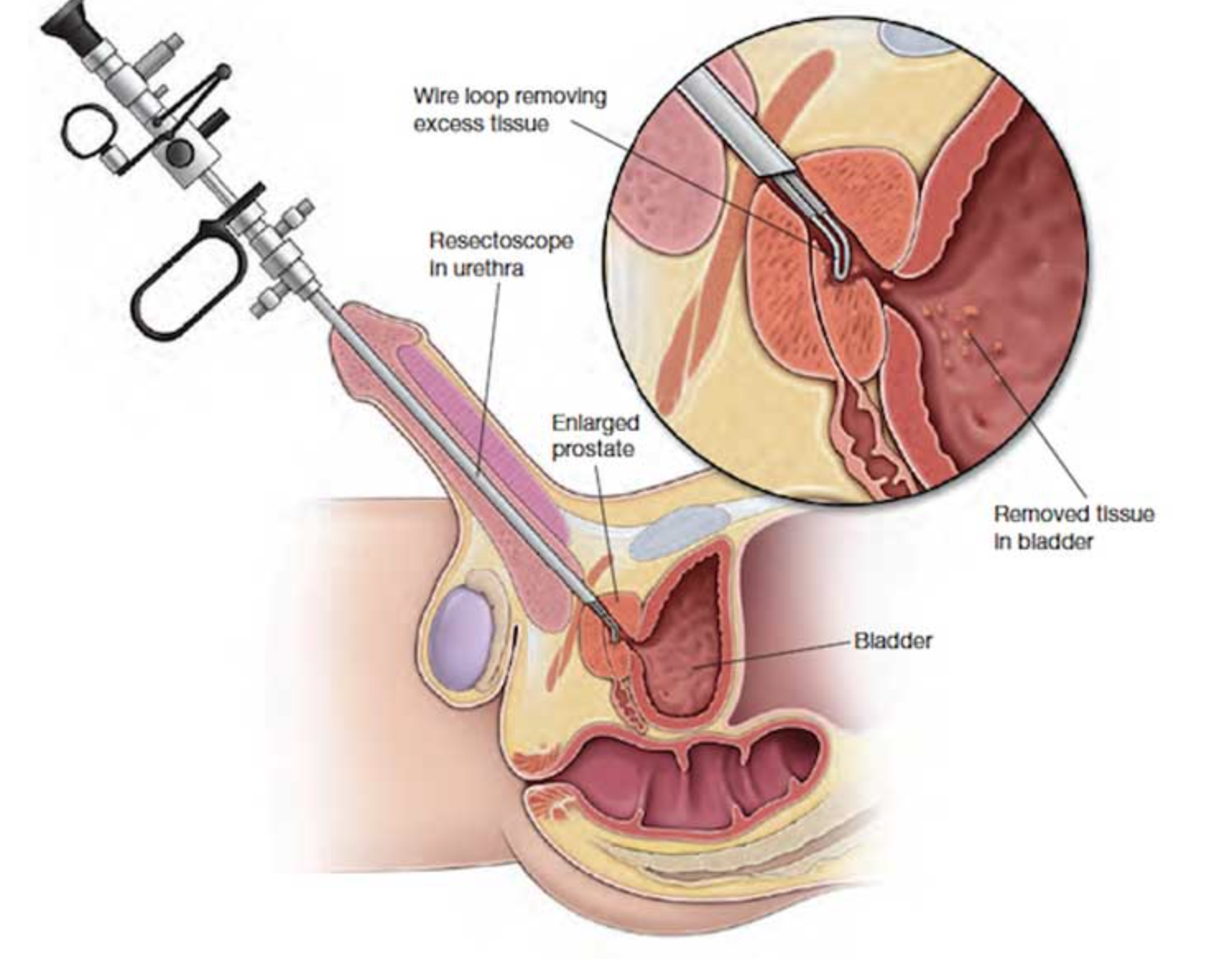
This means coring away part of the prostate to widen the urethra (tube between the bladder and the outside) and relive pressure on the bladder. The operation is done inside the urethra, so there are no cuts on skin.Under general / spinal anaesthetic, the surgeon passes a telescope (resectoscope) along the urethra and, using sterile fluid to fill the bladder, inspects the lining of the bladder to check if it is healthy. The resectoscope is then pulled back slightly until it is at the level of the prostate, and, using a high frequency electrical current wire loop, the surgeon takes small scoops from inside the prostate gland. When enough of the gland has been removed to open the urethra and bladder neck, the surgeon checks that bleeding has been controlled and flushes out the prostate chips. These are collected and sent for microscopic examination. A 3-way catheter (a tube passing along the penis to drain urine) is left in the bladder to enable constant flushing of the area to prevent clots forming. This is removed after a day or two. A catheter might be inserted straight into the bladder through the lower abdomen.
RISKS
These are the commoner risks. There may be other unusual risks that have not been listed here. Please ask you surgeon if you have any general or specific concerns.
There are risks associated with any anaesthetic.
You may have side effects from any drugs used. The commoner side effects include light-headedness, nausea, skin rash and constipation.
A transurethral resection of the prostate has the following general risks and limitations:
- You may get a urinary infection, requiring antibiotics.
- You may absorb fluid through the prostate bed during the operation and need drugs to help get rid of it.
- You may develop small areas of collapse in your lungs, which may require physiotherapy after the operation.
- You may develop a clot in your leg vein (deep vein thrombosis) with pain and swelling. If part of this breaks free, it may travel to the lungs (pulmonary embolism), causing shortness of breath. There is a small risk you could die from an embolism.
A transurethral resection of the prostate has the following specific risks and limitations:
- You may develop clots in the bladder after the operation, which may make it difficult to pass urine. Flushing the bladder through the catheter can wash these out.
- Rarely, you may need a blood transfusion because of heavier bleeding.
- After the catheter is removed your urine will burn and will be bloody. You will also have the sensation that you need to urinate frequently. This will continue to get better normally within the first week but can take up to 6 weeks
- You may still have some symptoms afterwards, particularly if the bladder has become overactive due to the blockage, or less commonly, weak due to long-lasting obstruction.
- You are likely to have retrograde ejaculation (i.e. the semen flows into the bladder during climax). This may prevent you from fathering children but will not affect your sexual functions in any other way.
- There is a small chance you may develop difficulties with erections for the first time after the operation. If your erections were normal before surgery, this risk is similar to that of erection problems that occur with age.
- The operation does not reduce or increase the risk of developing prostate cancer.
- You have an extremely small risk of becoming incontinent of urine after the operation in the long term. You may be incontinent of urine temporarily afterwards because your bladder may become overactive for a while.
- Urethral stricture or bladder neck stenosis can occur due to scarring after surgery
Some of the above risks are more likely if you smoke, are overweight, diabetic, have high blood pressure or have had previous heart disease.
