Cystectomy
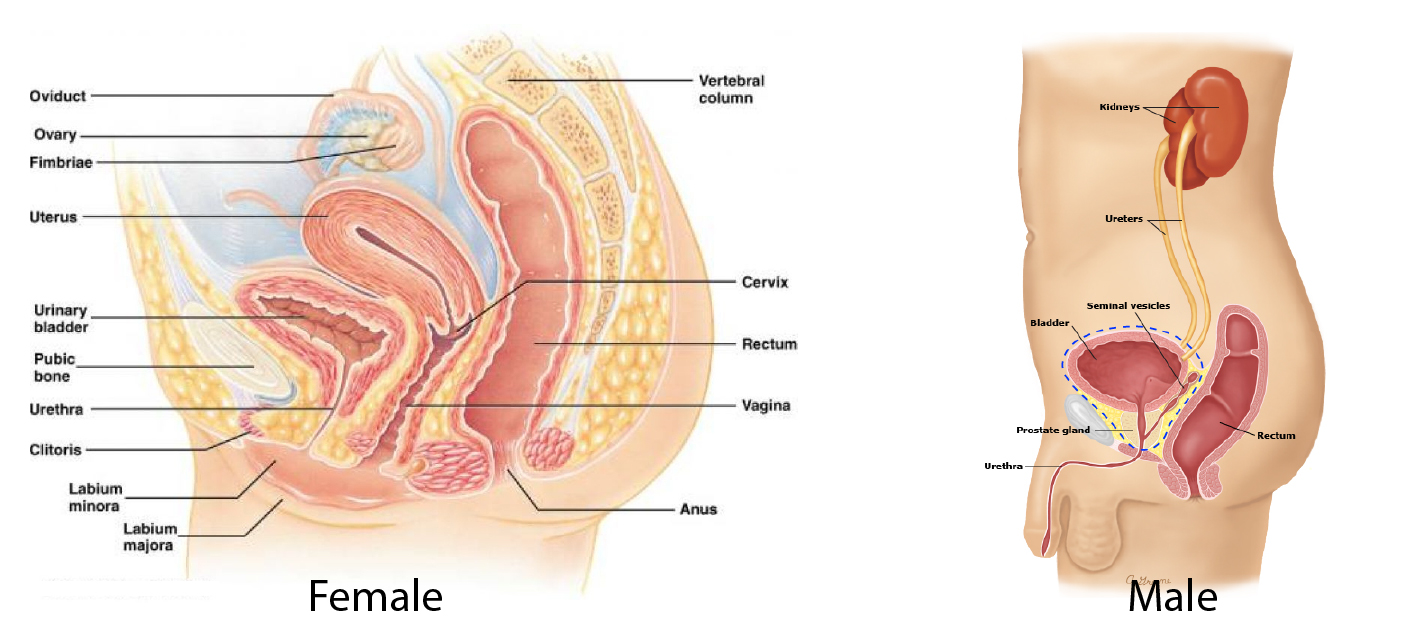
This means removing the bladder and its lymph nodes for cancer. In MEN, the prostate, seminal vesicles and part of the urethra may also be removed. In WOMEN, the cervix, womb, front wall of the vagina, and urethra may also be removed.
Under a general anaesthetic, the abdomen is opened through a midline cut and the ureters (tubes from the kidneys to the bladder) are identified. Small samples are sent for immediate microscopic examination to ensure there has been no spread of disease. The pelvic lymph nodes near the bladder may also be assessed and wide dissection of the lymph nodes may be necessary.
The bladder is then freed from its surrounding tissues and the urethra (tube from the bladder to the outside) is cut to allow the bladder to be removed and sent for examination. In WOMEN, the vagina is stitched closed.
Next a new way of draining urine to the outside is made. There are several options and your surgeon will explain if a different technique would be better for you. A short length of small bowel (ileum) is separated from rest of the bowel, the ureters are stitched to one end and the other end is brought out through the skin (stoma). The remaining bowel is reconnected.
A plastic bag is sealed to the skin around the stoma to collect the urine. Small suct
RISKS
These are the commoner risks. There may be other unusual risks that have not been listed here. Please ask you surgeon if you have any general or specific concerns.
There are risks associated with any anaesthetic.
You may have side effects from any drugs used. The commoner side effects include light-headedness, nausea, skin rash and constipation.
A radical cystectomy has the following specific risks and limitations:
- You may develop an abscess in the pelvis, with pain and fever. This may drain by itself, or may require a procedure guides by X-ray to locate the abscess.
- You may bleed heavily during the operation or afterwards. I may need transfusion, or rarely an operation.
- Your rectum (back passage) may be damaged during the operation. This will be repaired, but you may need temporary colostomy (bag) to allow the tissue to heal. The colostomy can usually be closed in several months’ time by doing a small operation.
- Loops of bowel may become stuck near the operation site during healing (adhesions). There is a small risk that irregular blockages of the bowel may follow, and these may sometimes require further surgery.
- Your cancer may reappear in the pelvis, or spread elsewhere at some time in future, despite the operation.
- You may develop a clot in a leg vein (deep vein thrombosis) with pain and swelling. If part of this breaks free, it may travel to the lungs (pulmonary embolism), causing shortness of breath. You could die from the embolism.
- You may develop salt imbalances as some urine components can be absorbed from an ileal conduit. This may require close monitoring and treatment. This may happen long after the operation.
- Your kidneys may fail as a result of repeated infections or stone blockage and you may need dialysis in future.
- You will be more prone to urinary tract infections and kidney stones and these may require treatment including antibiotics or surgery for stones.
- There is a risk the blood supply to the ileal conduit may fail. If this happens, a new conduit will need to be made in a second operation.
- The ureters may become scarred (stricture), reducing the drainage of urine form kidneys. Some strictures can be stretched open, but you may need another operation to refashion the join between ureter and the bowel.
- Your legs may swell because the lymphatic in your pelvis have been removed. This may be permanent or temporary and you may therefore be more prone to getting skin ulcers or infections.
Some of the above risks are more likely if you smoke, are overweight, diabetic, have high blood pressure or have had previous heart disease.
