ANTERIOR PROLAPSE REPAIR
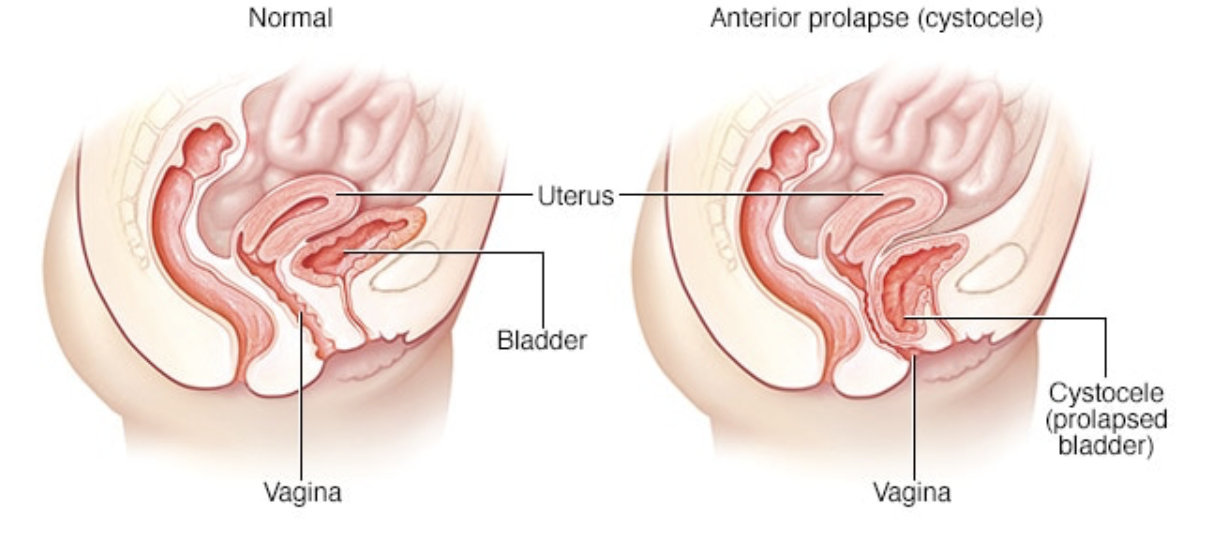
Anterior prolapse, also known as a cystocele, occurs when the supportive tissue between a woman's bladder and vaginal wall weakens and stretches, allowing the bladder to bulge into the vagina. Anterior prolapse is also called a prolapsed bladder.
Straining the muscles that support your pelvic organs may lead to anterior prolapse. Such straining occurs during vaginal childbirth or with chronic constipation, violent coughing or heavy lifting. Anterior prolapse also tends to cause problems after menopause, when estrogen levels decrease.
For a mild or moderate anterior prolapse, nonsurgical treatment is often effective. In more severe cases, surgery may be necessary to keep the vagina and other pelvic organs in their proper positions.
Your pelvic floor consists of muscles, ligaments and connective tissues that support your bladder and other pelvic organs. The connections between your pelvic floor muscles and ligaments can weaken over time, as a result of trauma from childbirth or chronic straining of pelvic floor muscles. When this happens, your bladder can slip down lower than normal and bulge into your vagina (anterior prolapse).
You will most likely remain in the hospital for 1 - 2 days after anterior vaginal wall repair. Your bladder may be affected by the surgery, and you may need to use a catheter for one to two days. A catheter is a small tube that’s placed in your bladder to remove urine from your body.
It’s common to be on a liquid diet after this surgery. Once you are able to urinate and have normal bowel movements, you can resume a regular diet.
RISKS
These are the commoner risks. There may be other unusual risks that have not been listed here. Please ask you surgeon if you have any general or specific concerns.There are risks associated with any anaesthetic, you may have side effects from any drugs used. The commoner side effects include light-headedness, nausea, skin rash and constipation.
Some potential adverse reactions related to surgical correction for anterior prolapse repair include:
Most often, the benefits of anterior vaginal wall repair outweigh the risks. In some cases, you may experience the following after surgery:
- painful urination
- a frequent, sudden urge to urinate
- a leakage of urine
- damage to your urethra, vagina, or bladder
Some of the above risks are more likely if you smoke, are overweight, diabetic, have high blood pressure or have had previous heart disease. Discuss these risks with your doctor before having an anterior vaginal wall repair.
Supporting your wound when coughing, sneezing or vomiting
Sit forward in a chair if possible. If in bed, bend your knees up. Place both hands over your wound, with your forearms resting firmly across the abdomen. It may help you to use a pillow across your abdomen as you cough, sneeze or vomit.
Mobilising correctly using your deep abdominal muscles
When you move from sitting to standing, and when you walk, try to gently
activate your deep abdominal muscles. Gently draw in the abdominal muscles
below your underwear. Placing your hands on your lower abdomen beneath
your navel will help you to check the activity of these muscles.
Moving in bed correctly
Slide one heel at a time along the bed towards your buttocks to bend both your knees. Keep
your head flat on the pillow. Lift your bottom off the bed as you push through your heels and
elbows to move yourself up the bed.
Positioning yourself to avoid straining your repair
When going to the toilet, remember to keep the curve in your back as you lean
forward at the hips. Lean your forearms or hands onto your knees
(refer to picture on right).
Upon discharge:
- You may have a watery blood-stained discharge for the first couple of weeks. As healing takes place you may experience some dark spotting as the internal sutures dissolve.
- You may feel fatigued.
- You may need to take some simple analgesia e.g. Panadol for pain or discomfort— especially on waking and settling at night.
What to avoid
- Avoid strenuous activity and heavy lifting for six to eight weeks.
- You should mobilise around the house and yard initially then go for short walks. Aim to gradually increase your activity everyday.
- Avoid sexual activity for six to eight weeks to allow time for healing to take place. Avoid straining when opening your bowels.
- Avoid constipation by eating a diet high in fibre and drinking two to three litres of fluid a day.
Please call the doctor if you experience any of the following:
- Severe pain
- Fever
- Heavy vaginal bleeding
- Vaginal discharge with an odour
- A lot of blood in your urine
- You have signs of infection (a burning sensation when you urinate, fever or chills)
