Kidney Stone manipulation: LASER
Kidney stones form in your kidneys. As stones move into your ureters (the thin tubes that allow urine to pass from your kidneys to your bladder) signs and symptoms can result. Signs and symptoms of kidney stones can include severe pain, nausea, vomiting, fever, chills and blood in your urine.
Laser lithotripsy is a procedure to break apart kidney stones in the urinary tract. It is done with a ureteroscope passed into the tubes of the urinary tract. Incisions are not needed.
The laser breaks the kidney stones into smaller pieces that can either be removed by the surgeon or pass out of the body in the urine.
A ureteroscope is an instrument with a long thin tube that is hollow like a straw. The doctor can use this scope to view the urinary tract, find kidney stones, and pass instruments to the stone.
The scope enters the urinary tract through the urethra, the tube that carries urine out of the body. The scope continues to pass through the urethra, bladder, and into the ureter or kidney (if necessary) to access the stone.
Once the doctor sees the stone, a fiber will be sent through the scope to the stone. The fiber can create a laser beam to break up the stone. Small pieces may be removed using a basket that is passed through the scope. Small sand-like pieces may remain and will be gradually passed through the urine.
A temporary stent may be placed in the ureter. The stent will keep the ureter open, improve urine flow, and help the stone pieces pass. The stent will be removed after a few days or weeks.
RISKS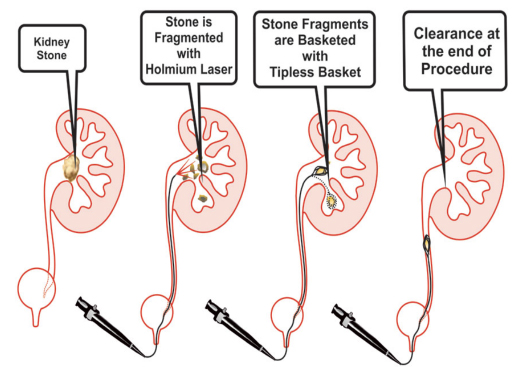
These are the commoner risks. There may be other
unusual risks that have not been listed here. Please
ask you surgeon if you have any general or specific
concerns. There are risks associated with any anaesthetic.
You may have side effects from any drugs used. The
Commoner side effects include light-headedness,
nausea, skin rash and constipation.
Factors that increase your risk of developing kidney stones include:
- Family or personal history. If someone in your family has kidney stones, you're more likely to develop stones, too. And if you've already had one or more kidney stones, you're at increased risk of developing another.
- Dehydration. Not drinking enough water each day can increase your risk of kidney stones. People who live in warm climates and those who sweat a lot may be at higher risk than others.
- Certain diets. Eating a diet that's high in protein, sodium (salt) and sugar may increase your risk of some types of kidney stones. This is especially true with a high-sodium diet. Too much salt in your diet increases the amount of calcium your kidneys must filter and significantly increases your risk of kidney stones.
- Being obese. High body mass index (BMI), large waist size and weight gain have been linked to an increased risk of kidney stones.
- Digestive diseases and surgery. Gastric bypass surgery, inflammatory bowel disease or chronic diarrhoea can cause changes in the digestive process that affect your absorption of calcium and water, increasing the levels of stone-forming substances in your urine.
- Other medical conditions. Diseases and conditions that may increase your risk of kidney stones include renal tubular acidosis, cystinuria, hyperparathyroidism, certain medications and some urinary tract infections.
Some of the above risks are more likely if you smoke, are overweight, diabetic, have high blood pressure or have had previous heart disease.
When you are discharged, take care of the following:
- You can continue with your normal daily activities (eg. Driving, sexual activities, walking, exercise & travel)
- Drink enough fluids (1-2 litres per day)
- Take your medicine as prescribed
- You can relax in a hot bath or shower if you experience discomfort
- Rest when you can
- If urine becomes blood stained, increase your fluid intake
- Make sure you attend to your follow-up appointment to remove the JJ-stent: usually within 2 weeks of stent placement if removed in theatre. +/- 2 day’s if to be removed in the rooms (your doctor will confirm whether it will be taken out in theatre or in the rooms)
- Contact your doctor if you experience any of the following:
- constant, unbearable, persistent pain;
- fever-like symptoms;
- nausea or vomiting;
- difficulty in passing urine;
- if your stent falls out;
- if you notice a significant increase of blood in the urine
You may reduce your risk of kidney stones if you:
- Drink water throughout the day. For people with a history of kidney stones, doctors usually recommend passing about 2.5 liters of urine a day. Your doctor may ask that you measure your urine output to make sure that you're drinking enough water. If you live in a hot, dry climate or you exercise frequently, you may need to drink even more water to produce enough urine. If your urine is light and clear, you're likely drinking enough water.
- Eat fewer oxalate-rich foods. If you tend to form calcium oxalate stones, your doctor may recommend restricting foods rich in oxalates. These include rhubarb, beets, okra, spinach, Swiss chard, sweet potatoes, nuts, tea, chocolate, black pepper and soy products.
- Choose a diet low in salt and animal protein. Reduce the amount of salt you eat and choose non-animal protein sources, such as legumes. Consider using a salt substitute.
- Continue eating calcium-rich foods, but use caution with calcium supplements. Calcium in food doesn't influence your risk of kidney stones. Continue eating calcium-rich foods unless your doctor advises otherwise. Ask your doctor before taking calcium supplements, as these have been linked to increased risk of kidney stones. You may reduce the risk by taking supplements with meals. Diets low in calcium can increase kidney stone formation in some people.
