POSTERIOR PROLAPSE REPAIR
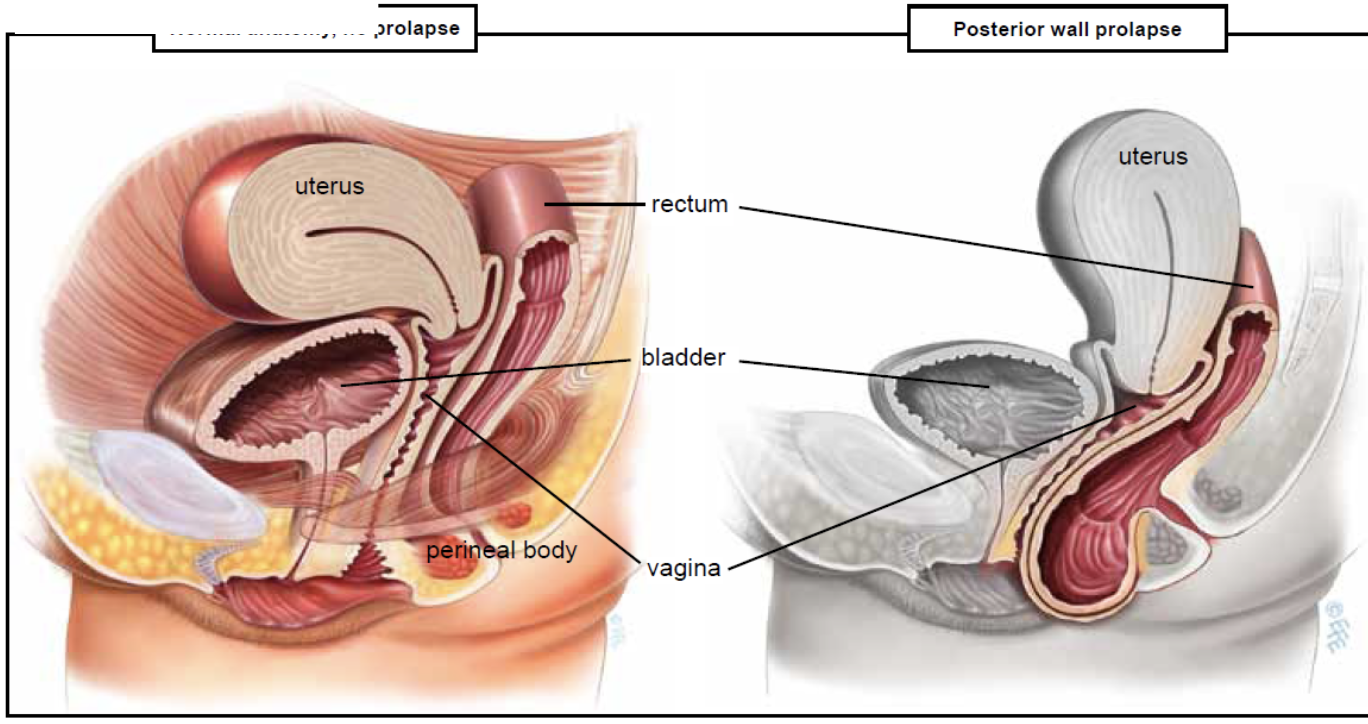
A posterior vaginal wall prolapse occurs when the thin wall of tissue that separates the rectum from the vagina weakens, allowing the vaginal wall to bulge. Posterior vaginal prolapse is also called a rectocele.
Childbirth and other processes that put pressure on pelvic tissues can lead to posterior vaginal prolapse. A small prolapse may cause no signs or symptoms.
If a posterior vaginal prolapse is large, it may create a noticeable bulge of tissue through the vaginal opening. This bulge may be uncomfortable, but it's rarely painful.
The muscles, ligaments and connective tissue that support your vagina become stretched and weakened during pregnancy, labour and delivery. The more pregnancies you have, the greater your chance of developing posterior vaginal prolapse.
The surgery uses a vaginal approach and usually consists of removing excess, stretched tissue that forms the posterior vaginal prolapse. A mesh patch might be inserted to support and strengthen the fascia. It’s common to be on a liquid diet after this surgery. Once you are able to urinate and have normal bowel movements, you can resume a regular diet.
RISKS
These are the commoner risks. There may be other unusual risks that have not been listed here. Please ask you surgeon if you have any general or specific concerns.
There are risks associated with any anaesthetic, you may have side effects from any drugs used. The commoner side effects include light-headedness, nausea, skin rash and constipation.
The following general complications can happen after any surgery:
- Bleeding. Serious bleeding requiring blood transfusion is unusual following vaginal surgery (less than 1%) Post operative infection. Although antibiotics are often given just before surgery and all attempts are made to keep surgery sterile, there is a small chance of developing an infection in the vagina or pelvis.
- Bladder infections. (Cystitis) occur in about 6% of women after surgery and are more common if a catheter has been used. Symptoms include burning or stinging when passing urine, urinary frequency and sometimes blood in the urine. Cystitis is usually easily treated by a course of antibiotics.
The following complications are more specifically related to posterior vaginal wall repair:
- Constipation is a common postoperative problem and your doctor may prescribe laxatives for this. Try to maintain a high fibre diet and drinking plenty of fluids helps as well.
- Some women develop pain or discomfort with intercourse. Whilst every effort is made to prevent this happening, it is sometimes unavoidable. Some women also find intercourse is more comfortable after their prolapse is repaired.
- Damage to the rectum during surgery is a very uncommon complication.
Some of the above risks are more likely if you smoke, are overweight, diabetic, have high blood pressure or have had previous heart disease. Discuss these risks with your doctor before having an anterior vaginal wall repair.
What to expect after surgery:
It is normal to get a creamy discharge for 4 to 6 weeks after surgery. This is due to the presence of stitches in the vagina; as the stitches absorb the discharge will gradually reduce. If the discharge has an offensive odour contact your doctor. You may get some blood stained discharge immediately after surgery or starting about a week after surgery. This blood is usually quite thin and old, brownish looking and is the result of the body breaking down blood trapped under the skin.
Upon discharge:
- You may have a watery blood-stained discharge for the first couple of weeks. As healing takes place you may experience some dark spotting as the internal sutures dissolve.
- You may feel fatigued.
- You may need to take some simple analgesia e.g. Panadol for pain or discomfort— especially on waking and settling at night.
When can I return to my usual routine?
In the early postoperative period you should avoid situations where excessive pressure is placed on the repair, i.e. lifting, straining, vigorous exercise, coughing and constipation. Maximal strength and healing around the repair occur at 3 months and care with heavy lifting >10kg needs to be taken until this time.
It is usually advisable to plan to take 2 to 6 weeks off work; your doctor can guide you as this will depend on your job type and the exact surgery you have had.
You should be able to drive and be fit enough for light activities such as short walks within 3 to 4 weeks of surgery.
You should wait five to six weeks before attempting sexual intercourse. Some women find using additional lubricant during intercourse is helpful. Lubricants can easily be bought at supermarkets or pharmacies.
Please call the doctor if you experience any of the following:
- Severe pain
- Fever
- Heavy vaginal bleeding
- Vaginal discharge with an odour
- A lot of blood in your urine
- You have signs of infection (a burning sensation when you urinate, fever or chills)
